
views
X
Research source
Depending on where you live, you also may be in an HMO through Medicaid Managed Care. The process for canceling Medicaid is different for each of these 3 types. Although Medicaid is administered by individual states, the process for cancellation of your coverage is roughly the same throughout the US.
Canceling MAGI Medicaid Coverage
Contact your state's health care department. Since Medicaid is administered by individual states, if you want to cancel your Medicaid coverage you need to go through your state's health care department. If you're not familiar with your state's offices, do a search online to find the main website. The website should have a toll-free number as well as a location directory for physical offices. You also may be able to find contact information on your Medicaid card.

Visit your state's marketplace website if you want to cancel online. If you have an account online on your state's health care marketplace website, you may be able to cancel your Medicaid coverage through that account. If you don't already have an account but want to cancel your Medicaid online, follow the prompts to set up an account first. Once your account is verified you should be able to use it to cancel your coverage.

Select the correct date for your coverage to end. When you cancel your Medicaid, it will end on the last day of the month in which you request that your coverage be terminated. Check the dates carefully, especially if you've gotten other health care coverage, to avoid a gap in coverage. For example, if you request cancellation of your Medicaid on December 7, your coverage will actually end on December 31.

Confirm cancellation of your coverage. You will receive a written notification in the mail to inform you that your Medicaid has been cancelled. It will include information on the last effective date of your coverage, and any other steps you need to take.

Report changed life circumstances if you no longer qualify for Medicaid. If you qualified for Medicaid because your MAGI was below the threshold set by the federal government, you are responsible for reporting any changes to the information you reported. These changes could result in you no longer being eligible for Medicaid coverage. If you are no longer eligible, your coverage will be cancelled. This could happen if, for example, you get married, or get a new job that pays more money than your old job. You may also have the option of simply ending your coverage, although typically you have to report changed circumstances as a reason to end your coverage. You can report online, over the phone, or by visiting a local Medicaid office in person.
Canceling Classic Medicaid Coverage

Determine why you qualified for Medicaid coverage. You have what may be referred to as "Classic" Medicaid or "Non-MAGI" Medicaid (depending on your state) if you qualified for Medicaid for some reason other than your income. For example, you may have qualified for Medicaid coverage because you are over 65, or because you have a disability, such as blindness.

Call or visit your state's Medicaid office. Going directly to your local Medicaid office often is the easiest way to cancel your coverage. You'll have the benefit of working with a trained staff member who can assess your situation and make sure your coverage is cancelled correctly. There may be contact information on your Medicaid card, or on any Medicaid statements you've received. You can also find contact information and addresses of local offices on the website of your state's health care department.

Use your marketplace account to cancel online. If you've set up an account on your state's health care marketplace website to manage your Medicaid, you may be able to cancel your coverage online. When you log in, look for a link to "Report changes" or "Edit your coverage." Click the link and follow the prompts to cancel your Medicaid coverage. When you cancel your coverage, check the final date that you'll be covered under Medicaid. If you now have other health insurance, you want to make sure there's no gap between when your Medicaid ends and your new coverage starts.

Check your mail for written notification of your cancellation. Once you've cancelled your Medicaid, your state Medicaid office will send you written confirmation of the cancellation. Review the notice and make sure all the information on it is correct and there's nothing else that you need to do to complete the cancellation.
Canceling Medicaid Managed Care
Check the date you were assigned to the HMO. If you were automatically assigned to an HMO, you only have a brief period of time (typically about 90 days) to disenroll from it or switch to a different plan. If you wait until after that 90-day period, you won't be able to get out of it unless you have an approved reason for needing to do so. For example, you could get out if the doctors didn't speak your language, or if their office was too far away from your home.
Call your state's health department. Your state's health department or Medicaid office will have a toll-free customer service number for you to call. This number may be on your Medicaid card, and will also be listed on any Medicaid notices you received. When you call, explain that you want to get out of your HMO and ask for a disenrollment form. They will mail the form to you.
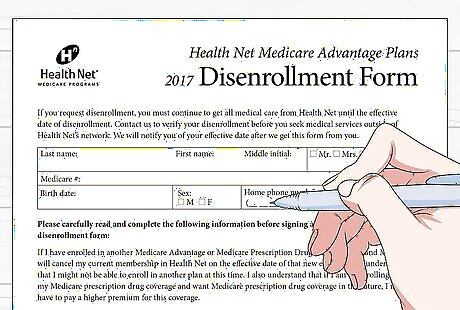
Fill out your disenrollment form. When you get the disenrollment form in the mail, fill it out immediately. You will need to provide personal identity information, such as your name and Social Security number. You also may be asked for the reason you're requesting disenrollment from the HMO. If you believe you are exempt or excluded from the HMO requirements, you may need to provide additional information.
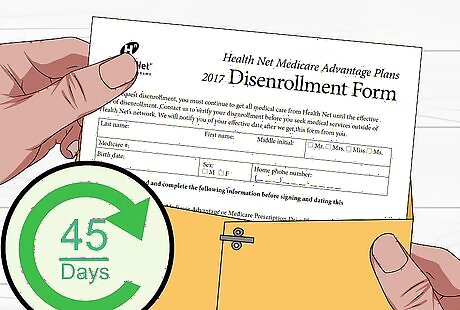
Submit your form as soon as possible. It can take as long as 45 days for your disenrollment to be processed. Especially if you are in the 90-day grace period, it's important to get your form to the state office as quickly as possible so they can start the process. If you need your disenrollment processed more quickly, you may be able to have your disenrollment expedited. Call your Medicaid office and tell them you need an expedited disenrollment form. Be prepared to tell them the reason you need expedited processing.
File an appeal if your request is denied. Your state's health care department and your HMO will review your request for disenrollment, and it may not be granted. If it is denied, you will receive a notice with the reasons why. Your notice will include instructions on how to appeal the decision. You only have a limited time to file your appeal, so if you plan to appeal the decision you should do so as soon as possible.


















Comments
0 comment