views
Treating Stress Incontinence at Home

Use the bathroom often. Trying to hold off on using the bathroom will lead to many more instances of leaks. Use the bathroom whenever you first feel the urge to go. Also, make sure you use the bathroom whenever you can if you’re going long distances between stops.
Treat any unresolved constipation. Constipation contributes to stress incontinence by increasing abdominal pressure and stimulating nerves near the rectum that increase urinary frequency. You can take simple steps at home to treat constipation, including: Eating more high-fiber fruits, vegetables, and grains Staying hydrated Staying physically active You can find more specific information at How to Regulate Bowel Movements

Eliminate foods and drinks that cause bladder irritation. A variety of foods and drinks can irritate your bladder or act as a diuretic (which means it makes you have to urinate more often). You may react to some but not all of these options. Try to isolate them in your diet to find out the ones that increase your stress incontinence. Some common options that increase stress incontinence include: Caffeine Carbonated beverages Citrus Chocolate Alcohol Spicy foods

Reduce fluid intake. If you still have occurrences after eliminating bladder-irritating beverages, then try to reduce your overall fluid intake; however, do not risk dehydrating yourself. Only reduce the amount of fluid you drink if you already drink more than the suggested eight to ten glasses of water a day. Reduce the amount of liquid that you are drinking after 4:00 if you are having problems in the evening and at night.

Quit smoking. In addition to a wide array or other health complications, smoking can also irritate your bladder, leading to overactive symptoms and increased incidence of stress incontinence. Many smokers also develop a chronic cough, which can cause more instances of leakage. Trying to stop smoking cold turkey rarely works for most smokers. Take advantage of available smoking cessation aids such as nicotine patches and gum, as well as support communities to taper off your tobacco addiction. You can find more information related to smoking cessation at How to Quit Smoking.

Get more exercise. Carrying extra weight can place increased pressure on your bladder and pelvic floor muscles. Professionals consider a body mass index (BMI) of 25 or higher overweight (with 30 meaning obese). Even the moderate loss of some excess weight can lead to dramatic improvement with symptoms. A great exercise routine for shedding extra pounds includes thirty minutes of moderate aerobic activity (such as brisk walking or cycling) five times a week. If you prefer high-intensity workouts (such as playing sports), then aim for seventy-five minutes a week. Note that weight training is not as effective at burning calories as aerobic exercise. In fact, chronic heavy lifting can increase stress incontinence by reducing the strength of your pelvic floor. Learn more about calculating your BMI at How to Calculate Your Body Mass Index (BMI). Some doctors suggest that you wear a tampon if you are having stress incontinence symptoms when you do exercise like running, as this increases support in the vagina. Remember not to leave you tampon in order to prevent toxic shock syndrome.

Balance your diet. Eating right is just as important to losing extra weight as exercise. Cut out processed foods, sugary foods and beverages, and sources high in saturated fat. Instead opt for a diet rich in fruits, vegetables, lean meats (fish and skinless chicken), and whole grains. Consult your doctor about the most effective changes you can make to your diet.
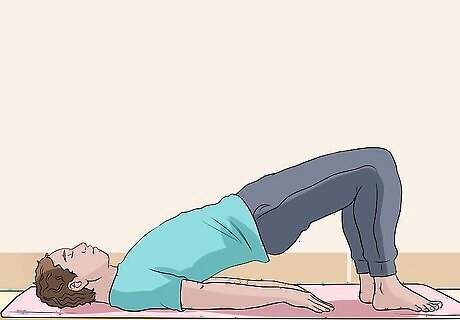
Strengthen your pelvic floor muscles. Weakened pelvic floor muscles (often from childbirth) are a leading cause of stress incontinence. Up to 75 percent of women with the condition have success with Kegel exercises to strengthen these muscles (though both men and women can do them). Have patience because it can take weeks or even months to show results. To perform Kegel exercises, isolate the muscles by intentionally stopping the flow of urine next time you go. Once you know what using those muscles feels like, hold them tight for an eight count before relaxing them while counting to ten. Do ten repetitions three times daily. You can also start with a lower count and increase it over time. You can also try vaginal weights, which are cone-shaped weights that you insert into your vagina like a tampon and help to strengthen the pelvic floor muscles. You will start with a low weight, holding it for one minute twice a day. Once you can hold that weight for 15 minutes, you move up to the next heaviest weight. Yoga has also been shown to strengthen the pelvic floor muscles. Postures like fish, pike, or crow work in the very same way as Kegel exercises.

Use tricks to reduce the amount of leakage. These steps take time. While you’re waiting for results, you can take other steps to reduce the appearance and amount of leakage you experience. You should: Cross your legs when you start laughing or feel a cough or sneeze coming on, which will help support your bladder and reduce pressure. Line your underwear with a stress incontinence product. These pads will stop any staining on your clothing and reduce odor. Tighten your Kegel muscles and buttocks when sitting to reduce other unintentional leakage.

Manage your blood sugar. If you’re diabetic, then changes in blood sugar can lead to increased incidence of stress incontinence. Monitor your blood sugar regularly and keep it under control by staying physically active and watching your diet.
Seeing Your Doctor to Treat Stress Incontinence
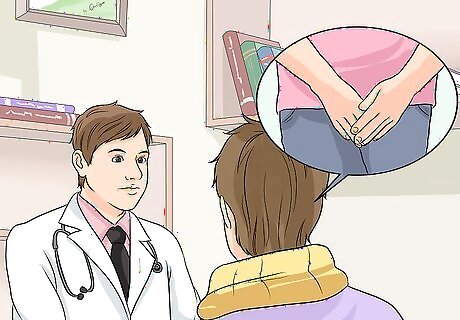
Recognize when to see your doctor. If your symptoms don’t improve from steps at home or if the leakage begins interfering with your activities of daily life, then make an appointment with your doctor. Your doctor will have a variety of steps available based on the severity and other specifics of your case, including both medications and surgical intervention in severe instances. Give your doctor a complete picture of your medical history and tell him what steps you’ve already tried.

Submit to any diagnostic testing. Your doctor will perform a physical examination of your abdomen and genitals, likely asking you to clench several muscles in the process. She may also want to run other diagnostic tests, which may include: Urine sample testing for infection, the presence of blood, or abnormalities that would increase the sensitivity or irritability of your bladder A neurological examination to identify any nerve damage in the pelvis A urinary stress test, during which the doctor will observe for urine loss while you cough or bear down Bladder function testing, which will measure the amount of urine left in the bladder after urination and pressure inside the bladder
Ask about medication options. Your doctor will likely encourage you to continue with home treatment steps (possibly even augmenting your routine). He may also recommend a medication to help reduce your stress incontinence. Medications that can help with mild to moderate cases include: Anticholinergic medicines—oxybutynin (Oxytrol, Ditropan), tolterodine (Detrol), and trospium (Sanctura)—to help relax the bladder muscles and reduce contractions and leakage Antimuscarinic drugs—atropine, solifenacin—to stop bladder contractions (may increase the amount of urine left in the bladder after emptying) Imipramine—a tricyclic antidepressant—that relaxes the bladder muscles to help with full evacuation Estrogen creams and vaginal tablets or rings that can help women who have gone through menopause to increase the strength of the pelvic floor muscles
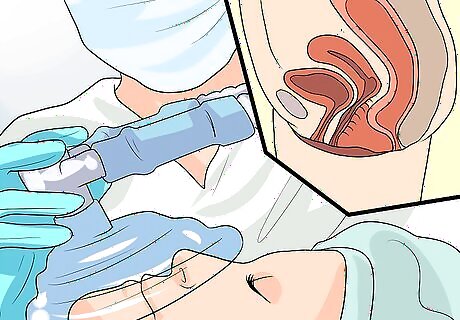
Consult your physician about surgical options. When all other options have failed to relieve your stress incontinence symptoms, your doctor may suggest surgical options as a last resort. Your doctor will base the recommendation of a specific procedure on your sex and other criteria. Options include: Anterior vaginal repair, which restores vaginal walls strength when bladder prolapse is involved (the bladder bulging into the vagina). Artificial urinary sphincter, which is a device used mainly in men to stop urine leakage. Collagen injections, which thicken the area around the urethra to reduce leakage. This option can require multiple procedures. Retropubic suspension, which is a procedure that lifts the bladder and urethra to reduce strain and pressure. Vaginal sling procedures, which support the urethra with the use of a sling to reduce strain and pressure.




















Comments
0 comment