
views
Preparing for the Birth

Call for help if possible. Contact emergency services. That way, even if you have to deliver the baby yourself, help will arrive soon if you experience complications. The dispatcher should also be able to either talk you through the delivery or connect you to someone who can. If the person in labor has a doctor or midwife, call them too. The medical professional can often stay on the phone and help guide you through the process.

Determine how far labor has progressed. The first stage of labor is called the “latent” stage, where the body is getting ready to deliver by dilating the cervix. It can take a long time, especially if this is the person's first child. The second, or “active” stage occurs when the cervix has completely dilated. People may not experience as much pain or discomfort during this stage as later stages. If the cervix is fully dilated, and you can see the baby's head crowning, they're in stage two. Wash your hands, skip to the next section and get ready to catch the baby. Unless you have been trained to do so, don't try to examine the cervix. Just watch to see if the head begins to appear.
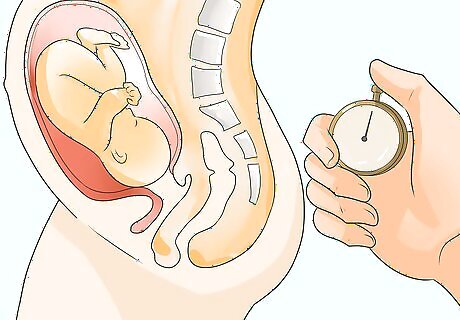
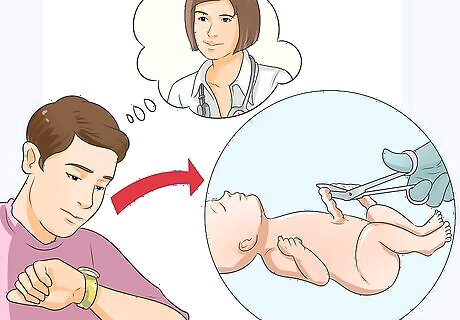
Time contractions. Time the contractions from the beginning of one to the beginning of the next, and note how long they last. The further along labor is, the more regular, stronger, and closer together contractions become. Here's what you need to know about contractions: Contractions that are 10 minutes apart or less are a sign that a person has entered labor. Physicians recommend that you contact the hospital when contractions are 5 minutes apart and last 60 seconds, and this activity has been going for an hour. If this is the case, you probably have time to make it to the hospital if you live close to one. First-time parents are likely to give birth when contractions are three to five minutes apart and last 40 to 90 seconds, increasing in strength and frequency for at least an hour. If the contractions are two minutes or less apart, buckle down and get ready to deliver the baby, especially if the person has given birth quickly in the past. Also, if the parent feels like they're going to have a bowel movement, the baby is probably moving through the birth canal, creating pressure on the rectum, and is on their way out. If the baby is preterm then you should contact the person's physician and emergency services at any signs of labor.

Sanitize your arms and hands. Remove any jewelry, such as rings or watches. Wash your hands thoroughly with antimicrobial soap and warm water. Scrub your arms all the way up to your elbows. If you have the time, wash your hands for five minutes; if you don't have time for that, wash them thoroughly for at least one minute. Remember to scrub in between your fingers and under your nails. Use a nail brush or even a toothbrush to clean under your nails. Wear sterile gloves if available. Don't wear things like dishwashing gloves, which are likely loaded with bacteria. To finish (or if you don't have access to soap and water), use an alcohol-based hand sanitizing product or rubbing alcohol to kill off any bacteria and viruses that may have been on your skin. This helps prevent giving the parent or the baby an infection.

Prepare a birthing area. Get set up so that you have everything you'll need within easy reach, and so the parent is as comfortable as possible. There will be a mess afterwards, so you may want to have the birthing area somewhere you don't mind getting messy. Collect clean towels and clean sheets. If you have clean waterproof tablecloths or a clean vinyl shower curtain, these are excellent at preventing blood and other fluids from staining furniture or carpeting. In a pinch, you can use newspapers, but they are not as sanitary. Get a blanket or something warm and soft to wrap the baby in. The infant must be kept warm once they are delivered. Find a few pillows. You might need them to prop up the parent as they're pushing. Cover the pillows with clean sheets or towels. Fill a clean bowl with warm water and get a pair of scissors, a few lengths of string, rubbing alcohol, cotton balls, and a bulb syringe. You may find that sanitary napkins or paper towels are helpful to stop the bleeding later. Get a bucket in case the parent feels nauseated or the need to vomit. You may also want to get a glass of water for them. Labor is hard work.

Help the person in labor stay calm. They may feel panicky, rushed, or embarrassed. Do your best to remain calm and reassuring to help them relax. Ask the parent to undress from the waist down. Provide them with a clean sheet or towel to cover up, if they'd like. Encourage them to breathe. Avoid hyperventilation by speaking in a low, soothing voice and verbally directing their breathing. Encourage them to inhale through the nose and out through the mouth in an even, rhythmic manner. If you're still having trouble, hold their hand and take deep, slow breaths along with them. Reassure them. This is probably not the birthing experience they had in mind, and they might be worried about potential complications. Tell them that help is on the way, and that you'll do the best you can in the meantime. Remind them that people have given birth outside of hospitals for thousands of years, and that it's more than possible to come through it safely. Validate them. The expectant parent may feel scared, angry, giddy, or any combination of those feelings. Validate whatever they are feeling. Don't try to correct them or argue with them.

Help the person find a comfortable position. They might want to walk around or crouch down during this stage of labor, especially when a contraction hits. As they start to transition to the second phase, they might want to settle into a position to give birth or cycle through a few different ones. Switching between positions may help the labor progress more smoothly, but let them decide what's working for their body. Here are four standard positions, and the pros and cons of each: Squatting. This takes advantage of gravity, and can open the birth canal 20%-30% more than other positions. If you suspect the baby is breech (emerging feet-first), suggest this position as it gives the baby room to rotate. You can help the parent in this position by kneeling behind them and supporting their back. All-fours: This position is gravity-neutral and can ease back pain, and the person might instinctively choose it. It can provide pain relief if they have hemorrhoids. Position yourself behind them if that's the case. Side-lying: This leads to a slower descent through the birth canal, but can lead to a more gentle stretching of the perineum and may reduce tearing. Have the parent lie on their side, with their knees bent, and lift the top leg. They might also need to prop themself up on an elbow. Lithotomy position (lying back). This is the most common position used in hospitals, with the patient lying flat on their back and their legs bent at the knee. It allows maximum access for the caregiver, but it puts a lot of pressure on the patient's back and is not considered ideal. It also may make contractions slower and more painful. If the person in labor seems to prefer this position, try putting a few pillows under their back to ease the pain.
Delivering the Baby

Guide them in pushing. Don't encourage them to push until they feel an unstoppable pressure to do so — you don't want to waste their energy and make them exhausted too early. When they are ready to push, they may feel increased pressure near their lower back, perineum, or rectum. It may even feel to them as though they are ready to have a bowel movement. When they are ready, you can guide them through the pushing. Ask the parent to curl forward and tuck their chin. This curved position will help the baby through the pelvis. When pushing, it can be helpful if the parent holds their knees or legs with their hands and pulls their legs back. The area around the vagina will bulge until you see the top of the baby's head (crowning). As soon as the baby crowns, it's time for the parent to push in earnest. Encourage them to focus their abdominal muscles to push down, as you might do when you're trying to urinate faster or have a bowel movement. This can help avoid straining or directing the pushing force upward toward the neck and face. Three to four pushes, lasting 6-8 seconds each, are considered appropriate per contraction. However, it is important to encourage the parent to do whatever comes naturally to them. Keep encouraging deep, slow breathing. Pain can be controlled to different extents through mental relaxation and by concentrating on deep breathing instead of panicking or being distracted by everything that is going on. Different people have different levels of mental control, but deep, slow breathing is always a benefit during childbirth. Understand that the person may urinate or have a bowel movement during labor. This is normal and is not a cause for concern. Don't even bother mentioning it -- you don't want to embarrass them.

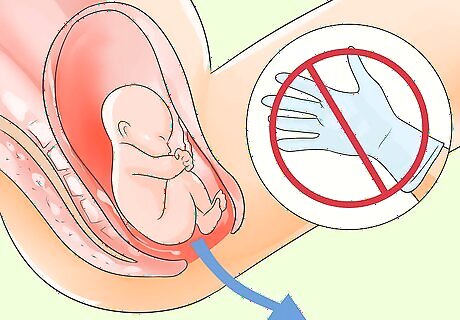
Support the baby's head as it emerges. This step isn't complicated, but it's important. Pay extra attention to these tips: Do not pull on the baby's head or the umbilical cord. This can cause nerve damage. If the cord is wrapped around the baby's neck, which is fairly common, gently lift it over the baby's head or carefully loosen it so the baby can slip through the loop. Do not pull on the cord. It's natural for the baby to pass through the pelvis face-down. If the baby's face is facing toward the parent's back, don't worry. This is actually the best position for delivery. If you see the feet or buttocks coming first (rather than the head), you have a breech birth. See instructions for that situation below.
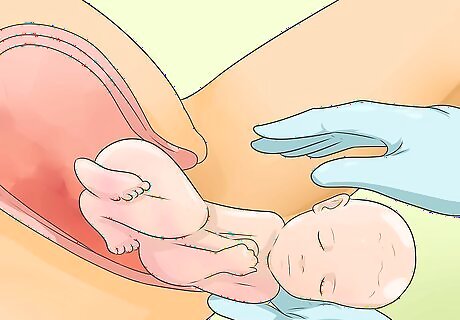
Prepare for the baby's body to emerge. When the baby's head rotates to one side (which they will probably do on their own), be prepared for the body to come out with the next push. If the baby's head does not rotate to one side, ask the mother to push again. The baby will likely rotate spontaneously. If the baby's head doesn't rotate without help, gently turn it to one side. This should help a shoulder emerge with the next push. Don't push it if you feel any resistance. Deliver the other shoulder. Gently lift the body toward the parent's stomach to help the other shoulder come through. The rest of the body should follow quickly. Keep supporting the head. The body will be slippery. Make sure you're still providing enough support for the baby's neck, which isn't strong enough to support the head on its own.

Manage complications. Hopefully, all goes well, and you've successfully delivered a healthy baby by now. If the delivery seems stalled, though, here's what you can do: If the head comes out, and the rest of the body doesn't come out after the parent pushes three times, have them lie on her back. Instruct them to grab their knees and pull their thighs toward their stomach and chest. This is called the McRoberts position, and it's very effective at helping push the baby out. Have her push hard with each contraction. Never push on a mother's abdomen to try to help deliver a stuck baby. If the feet come out first, see the section on breech birth below. If the baby is still stuck and paramedics are still nowhere near the scene, you can try to guide the baby's head gently downward toward the parent rectum. This should only be attempted as a last resort, and should not be attempted at all if medical attention will be arriving soon.

Hold the baby so the fluids in their mouth and nose drain. Hold the delivered baby with two hands, one supporting their neck and head. Tilt the head down at about a 45-degree angle to allow the fluids to drain. The feet should be slightly above the head (but don't hold the baby by the feet). You can also wipe any mucus or amniotic fluid from the nose and mouth area with clean, sterile gauze or cloth.

Place the baby on the parent's chest. Ensure full-skin contact, and cover them both with clean towels or blankets. The skin-to-skin contact encourages a hormone called oxytocin, which will help the parent deliver the placenta and bond with the baby. Position the baby so that their head is still slightly lower than the rest of the body, so fluids can keep draining. If the parent is lying down and the baby's head is on their shoulder, and their body is on their breast, this should happen naturally.
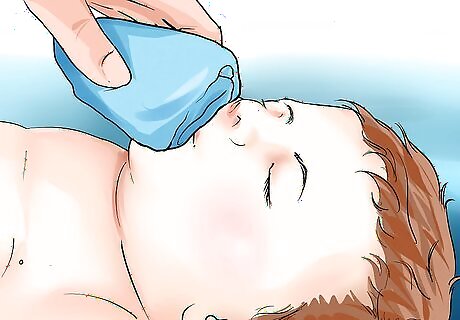
Make sure the baby is breathing. They should be crying slightly. If they're not, you can take a few steps to help make sure the airway is clear. Rub the body. Physical touch will help the baby breathe. Rub over their back firmly with a blanket while they're still on its mother's chest. If that's not helping, turn the baby so that they're facing the ceiling, tilt the head back to straighten the airway, and keep rubbing the body. They might not cry, but doing this ensures that the baby gets the air they need. Rubbing vigorously with a clean towel can also help stimulate the baby to breathe. Manually clear fluids. If the baby gags or turns blue, wipe fluids out of the mouth and nose with a clean blanket or cloth. If that doesn't do the trick, squeeze the air out of a bulb syringe, put the tip in the nose or mouth, and release the bulb to suck the fluid into the bulb. Repeat until all the fluid is cleared, emptying the bulb between uses. If you don't have a bulb, you can use a drinking straw. If nothing else has worked, try flicking the soles of the baby's feet with your fingers, or gently popping their bottom. Don't slap the baby. If none of this helps, perform infant CPR.
Delivering a Breech Birth
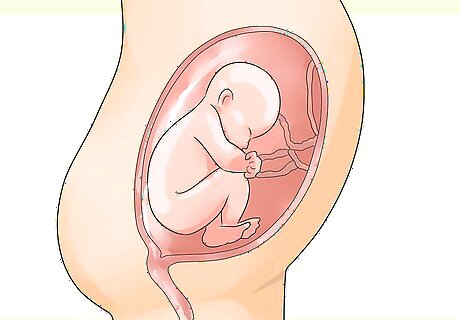
Know that a breech birth is unlikely. If it happens, a breech birth is a circumstance where the feet or buttocks enter the pelvis first instead of the head coming out.

Position the parent. Have them sit at the edge of a bed or other surface and pull their legs to their chest. As a precaution, put down pillows or blankets where the baby is likely to fall.
Do not touch the baby until the head comes out. You'll see their back and bottom hang down, and you'll want to grab it, but don't. Avoid touching the baby until the head is delivered because your touch could stimulate the baby to gasp while the head is still submerged in amniotic fluid. Make sure the room is warm, as a drop in temperature could also cause the baby to gasp.

Catch the baby. Once the head is delivered, grab the baby under their arms and bring them up to the parent. If the head doesn't come out in the push after the arms come out, have the parent squat and push.
Delivering the Placenta
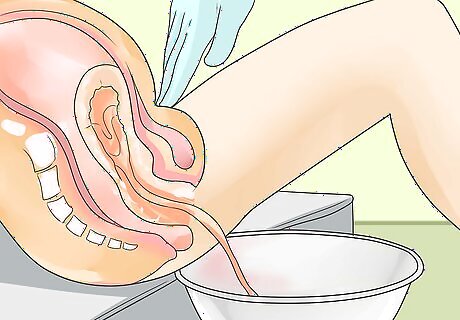
Prepare for the placenta. Delivering the placenta is the third stage of labor. It will arrive anywhere between a few minutes to an hour after the baby is delivered. The parent will probably feel an urge to push after a few minutes; this is helpful. Put a bowl close to the vagina. Right before it emerges, blood will come out of the vagina, and the cord will get longer. Have the parent sit up and push the placenta into the bowl. Rub their stomach below the belly button firmly to help slow down the bleeding. It might hurt, but it's necessary. Keep rubbing until the uterus feels like a large grapefruit in the lower belly.

Let the baby breastfeed. If the cord isn't stretched too tightly by doing so, encourage the parent to breastfeed as soon as possible. This will help stimulate a contraction and encourage the delivery of the placenta. It may also help slow bleeding. If breastfeeding isn't an option, stimulating the nipples can also help stimulate delivering the placenta.
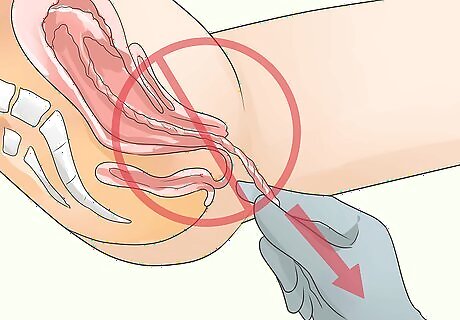
Don't pull on the umbilical cord. As the placenta is delivering, don't tug on the cord to hurry it along. Let it come out on its own as the person pushes. Pulling on it could cause severe damage.

Bag the placenta. Once the placenta is out, place it in a disposable bag or a container with a lid. Do not throw it out. When and if the person goes to a hospital, the doctor might want to inspect the placenta for any abnormalities.
Decide whether to cut the cord. You should only cut the umbilical cord if professional medical attention is hours away. Otherwise, leave it alone and just make sure it's not pulled tight. If you do need to cut the cord, first feel the cord gently for a pulse. After about ten minutes, the cord will stop pulsing because the placenta has separated. Don't cut it before then. Don't worry about pain. There are no nerve endings in an umbilical cord; neither parent nor child will feel pain when its cut. The cord will, however, be slippery and difficult to handle. Tie a string or lace around the cord, about three inches from the baby's belly button. Tie it tightly with a double knot. Tie another lace about two inches away from the first one, again using a double knot. Using a sterile knife or scissors (that have been boiled in water for 20 minutes or wiped down with rubbing alcohol), cut between the two laces. Don't be surprised if it's rubbery and tough to cut; just take your time. Cover the baby again when the cord is cut.
Caring for the Parent and Baby

Keep the parent and baby warm and comfortable. Cover them both in blankets, and encourage the parent to keep the baby on their chest. Replace any wet or dirty bedding, and move them to a clean, dry area. Control pain. Put an ice pack on the person's vagina for the first 24 hours to ease soreness and pain. Offer them acetaminophen/paracetamol or ibuprofen if they're not allergic. Give the parent something light to eat and a drink. Avoid carbonated drinks and fatty or sugary foods, as these could cause nausea. Toast, crackers, or light sandwiches are good options. The parent may want to rehydrate with an electrolyte-containing sports drink. Put a diaper on the baby. Make sure it's below the umbilical cord. If the cut cord smells bad (signaling an infection) clean it with alcohol until it doesn't smell anymore. If you have a small hat available, put it on the baby, so they don't catch a chill.

Massage the uterus through the abdomen. Sometimes, unexpected deliveries can cause hemorrhaging after delivery. It occurs in up to 18% of all deliveries. To help prevent this, you can firmly massage the uterus. If you see significant blood flow after the placenta is delivered, do the following: Place one (clean) hand inside the vagina. Place your other hand low on the parent's abdomen. Push down with the hand placed on the abdomen as you push against the uterus from the inside with the other hand. You can also make firm, repetitive squeezing movements with on hand on the lower abdomen without placing a hand inside the vagina.
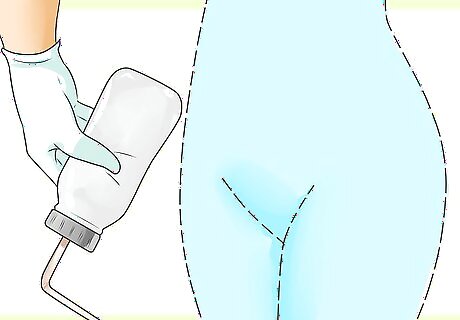
Prevent infection while going to the bathroom. Instruct and if necessary help the person pour warm water over the vagina every time they urinate to keep the area clean. You can use a clean squeeze bottle to do this. If they need to have a bowel movement, have them place a clean pad or washcloth against their vagina while they push. Help the person urinate. It is good for them to empty their bladder, but due to blood loss, it may be best to have them urinate in a pan or on a cloth you can move from under them, so they do not have to get up.
Get medical attention as quickly as possible. Once delivery is complete, proceed to the nearest hospital or await the ambulance you called.


















Comments
0 comment