views
Lifestyle Changes
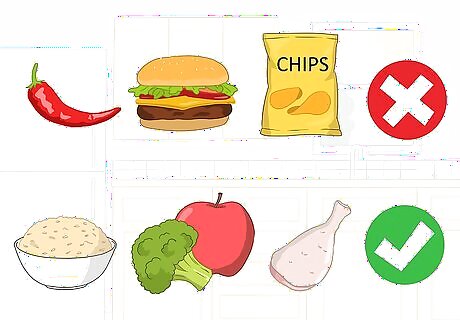
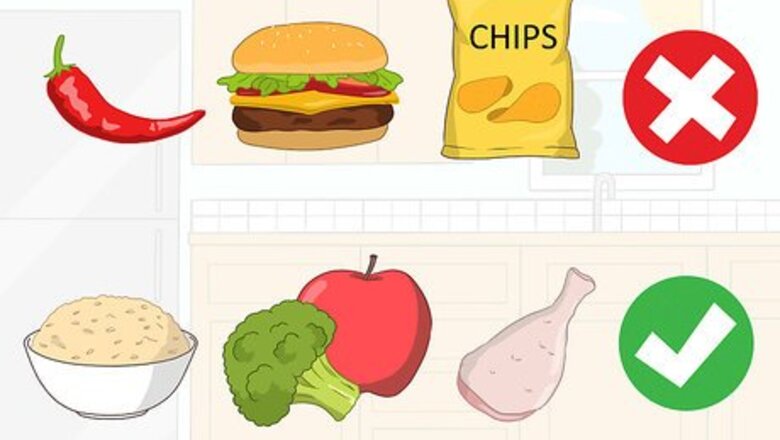
Eat a balanced diet. Taking care of your diet will keep any stomach and digestive symptoms at bay. Simply avoiding spicy food, junk food and fatty food will give you a healthier digestive system that is less prone to problems. Opt for more whole grains, leafy green vegetables, fruits, and lean meats. Adding fibers and cereal food to your diet will help to prevent constipation, which can irritate a fistula. Try noticing what types of food you are allergic to or that upset your stomach. Remember that it’s not always a stiff rule — each person is different. Fatty waste can increase the possibilities of blocking an anal fistula tunnel and thus can induce the formation of perianal abscess, the major cause of pain in people suffering from fistulas.

Drink more water. It is recommended to drink one and a half liters of water a day unless your doctor says otherwise. Stop drinking alcohol and soda; instead consume larger amounts of water and fruit juice. This will help prevent any possible occurrence of constipation, which puts pressure on your fistula. Excess water will make waste softer and will help clean the intestines; this is why if you drink excess amounts of water you will need to use the toilet more often. Water also prevents the intestines from getting blocked especially in patients suffering of some digestive diseases like Crohn’s disease, toxic megacolon, etc.
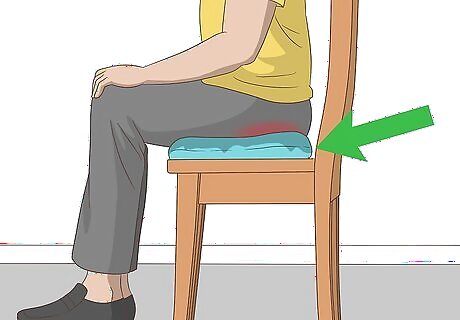
Use pillows. If your work forces you to sit down for many hours, avoid putting extra pressure on your back, butt, and legs, especially if you have an anal fistula. This could be done by sitting on a pillow or a “donut pillow” instead of the regular chair. Do what you can to feel comfortable. Try to avoid situations where you can foresee being uncomfortable or bring a pillow or other aid with you.
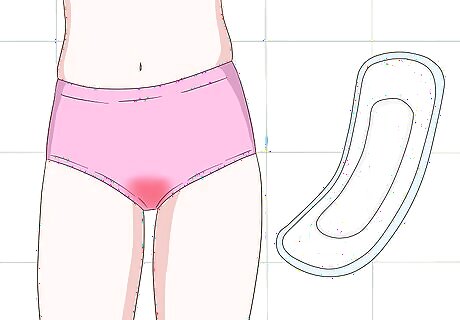
Use absorbent pads. If your fistula is resulting in unfortunate leakage down there, wearing soft, absorbent pads will help stop the issue. Adult diapers work, too, they're just a little bulkier and more stigmatized. Pads are thinner and much easier to deal with. Change the pads often as well since the discharge will have an unpleasant odor.
Maintain good personal hygiene. Make sure to wash yourself after each bowel movement or going to the toilet. Avoiding any bacteria remaining on your skin is the first step to avoiding an infection. This goes double in public restrooms and when you're experiencing leakage. If you’re outside and can’t do this, always keep wipes with you to be used instead until you can get home. Your hands experience have the most exposure to germs and therefore must stay clean. Change your underwear as needed throughout the day if the fistula is leaking. Change towels each time you bathe, too. Both of these prevent the spread of germs and growth of bacteria which can reduce perianal irritation and thus will help in eliminating the annoying symptoms people with fistula suffer from.
Take painkillers. Anorectal fistulas are often accompanied by pain that is constant, throbbing and that worsens severely when you are sitting down. To deal with this, talk to your doctor about what type of pain medication and dosage is right for you. Ibuprofen, a non-steroid anti-inflammatory (NSAID), may be helpful for treating fistula pain, or you may need a prescription medication. Pain may be a complication of fistula. A blocked tunnel will fill up instead of draining pus out — a process that may lead to the formation of an abscess, or a sack of pus near the skin surface. Pain also can be accompanied with an irritating sensation and redness that looks similar to diaper rash around the perianal skin because of the pus draining.
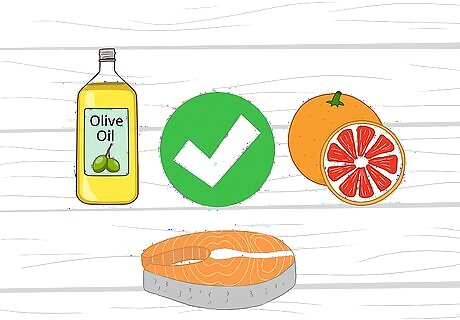
Strengthen your immune system. Maintaining a healthy diet and eating food rich in omega-3s, omega-6s, and vitamin C, like fish, olive oil and citrus fruits will help strengthen the immune system and decrease the levels of inflammation you may suffer due to a fistula. You may also take a supplement if your doctor feels it's wise. Exercise, drinking lots of water, sleeping well, and staying hygienic are also great strides you can make toward a healthier you. And if you have any bad habits — like smoking — consider this a reason to quit.

Stay active. If your condition allows for simple, gentle exercising such as slow walking, do so for your health and to aid in eliminating stress. Being stressed can affect your general mood and can trigger problems and irritate your stomach. This then affects your digestive system and your dietary habits on the whole, which creates a vicious cycle. Always stop and catch your breath for a while if you feel any pain or inability to continue. This is your body telling you it cannot handle the exertion you're putting it under. Ask your doctor for any kinds of light sports or exercises that you can do. Even at home, yoga is advised by many doctors to clarify your mind, removing stress, and fighting depression. It also enhances your mood and health in general.
Treatment
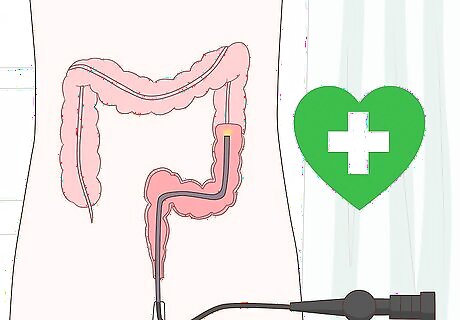
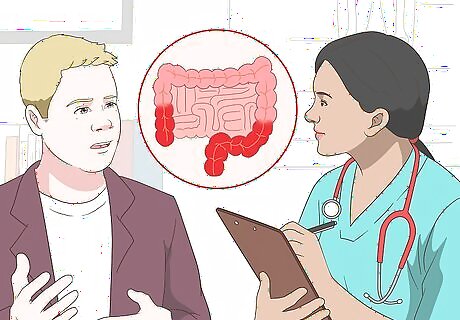
Visit your doctor. Diagnosis is by visual examination. A sigmoidoscopy must always follow the visual examination to rule out Crohn's disease, cancer, and other serious conditions. However, to know the ins and outs of your case, your doctor may conduct 1 or more of the following tests, too: Computerized Tomography (CT scan). Especially in patients with Crohn’s disease, a CT scan indicates the inflammatory stage before the possible formation of a fistula, in addition to showing the cavities of abscess to determine if surgical care is needed. Magnetic Resonance Imaging (MRI). This a helpful method to determine any enteric fistulas by revealing any inflammatory changes or accumulation of fluids in the fistula tube. Fistulography. This is an X-ray method in which a contrast media is injected at the external site of a fistula to clarify the fistula path and how deep it is through the tissues which will help in choosing the treatment. Ultrasonography. This combined with physical examination can be used to identify any presence of abscess or fluid accumulation that may reside in the fistula tube. Cystoscopy. This is useful for the “enterovesical fistula” that connects the intestine with the bladder. Microbiological tests. To indicate any sign of infection, especially in the presence of abscess, a urine culture may be required in case of colovesical fistulas.

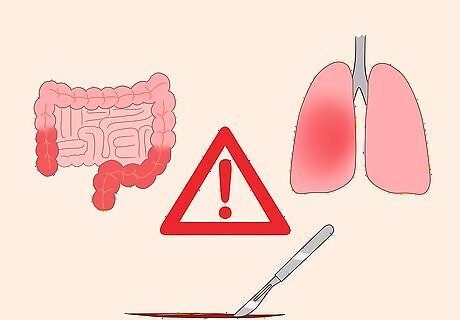
Undergo surgery. The most common treatment of fistulas is surgical care, which is called “fistulotomy." This process will remove the fistula and any pus or fluid gathering in it. Fistulotomy is effective in more than 85% of cases. In fistulotomy for rectal fistulas, a procedure called endorectal flap will be used. This is where the surrounding healthy tissues get put inside the fistula cavity to ensure the prevention of its blockage by feces in case of a recurrent infection. A seton stitch (passing a cord into the fistula in order to keep it closed during the drainage) is also reported to be used in fistulotomy. This, however, usually takes multiple visits to your doctor until recovery and eventually the stitches dissolve. There is a "Cutting Seton Treatment" known as "Kshar Sutra Therapy," which has a high success rate.
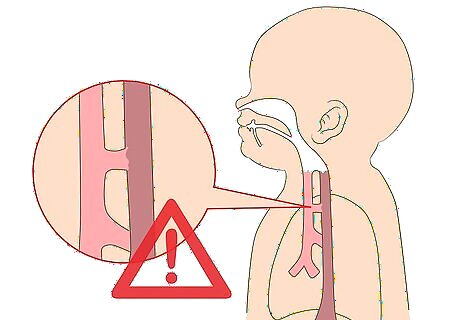
Take extra caution if you have a fistula near your esophagus. Fistulas between the esophagus and trachea-bronchial tree are considered life threatening and require immediate and ongoing treatment. If left untreated they can induce chronic lung abscesses and deadly pneumonia. Treatment is provided by a number of medical procedures such as: Esophageal dilation. This may last for months or even years in some patients. Flexible-metal mesh stents. These are the most effective in maintaining esophageal patency and structure. Plastic coated mesh stents. These can also be used to occlude trachea-esophageal fistulas; some are powered with a valve that prevents reflux when the fistula is located near the esophageal sphincter.
Follow up with your doctor. It’s incredibly important that you follow up with your doctor post-surgery, especially if you have a chronic inflammatory disease, such as Crohn’s disease or other conditions. In these cases, fistulas are just a side effect and the actual cause needs to be addressed. There are other issues that are related directly to intestinal fistulas that the affected patient must follow up on and be aware of, too. They must avoid sepsis by treating any signs of infections, such as inflammations in the tissues surrounding the fistula, control the drainage of the fistula and keep good care of the skin to maintain the nearby tissues in a healthy state. A gastrostomy tube may be required to feed someone with an esophageal fistula. This goes in through the abdominal wall and directly into the stomach. If needed, the tube would be placed while the patient is under anesthesia so they will not be in pain.
Talk to your doctor about taking antibiotics. Antibiotics may minimize the chances of forming any infections at the fistula site, especially for the enteric kinds. Elevated levels of white blood cells indicates the presence of an infection that may need to be treated with a suitable antibiotic. Fistulas can be treated initially with a compound treatment of metronidazole and ciprofloxacin or vancomycin. Metronidazole will be 250-500mg every 8 hours; Vancomycin is 125-250 mg every 6 hours, or three times daily one hour after eating.
Understanding Fistulas
Know the causes and predisposing factors. Most cases are related to chronic inflammatory diseases such as Crohn's disease and tuberculosis. Others may result from diverticulitis, tumors, or chronic trauma. A surgery or an injury can lead to the production of a fistula, too, as in the case of biliary or arteriovenous fistulas. Recto-vaginal fistulas may be secondary to Crohn's disease, obstetric injuries due to birth, radiation therapy or cancer. Fistulas in children or infants are mostly congenital affecting boys more than girls.

Know the signs and symptoms. Any fistula generally comes accompanied by these symptoms: Constant discharge (pus) Pain (related to infection) Bleeding Pain in the abdomen Diarrhea Loss of appetite Weight loss Nausea and vomiting
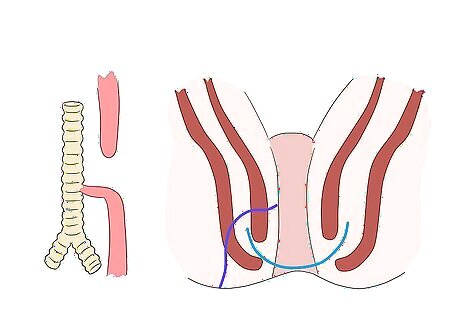
Know the different types of fistulas. A fistula, by definition, is a tube-like tunnel with 2 openings: 1 primary opening leading to another exterior opening called the secondary opening. Many types of fistulas are known, but 90% of all fistulas are anorectal fistulas. Physically, they can take on the following forms: Blind Fistula: A link between two surfaces; one end is closed and the other is opened. This can turn into a complete fistula if untreated. Incomplete Fistula: A link has only one external opening. Complete Fistula: A link between an internal opening and external opening. Horseshoe Fistula: A link in a U shape, between two external openings around the anus.
Know the complications of an anal fistula. Unfortunately, a fistula's symptoms isn't where the problem stops — it can also lead to its own complications. They are the following: Secretions that produce inflammation around the anal area Tumors of the anal canal Radial fungus disease (very rare) Exposure to severe trauma Cracks around the anal area Infections of the digestive tract Because of this, it is highly advised that you clean the anus well after using the toilet, observe the rules of public safety and personal hygiene, and use wipes after using the toilet and throw away after each use.



















Comments
0 comment