views
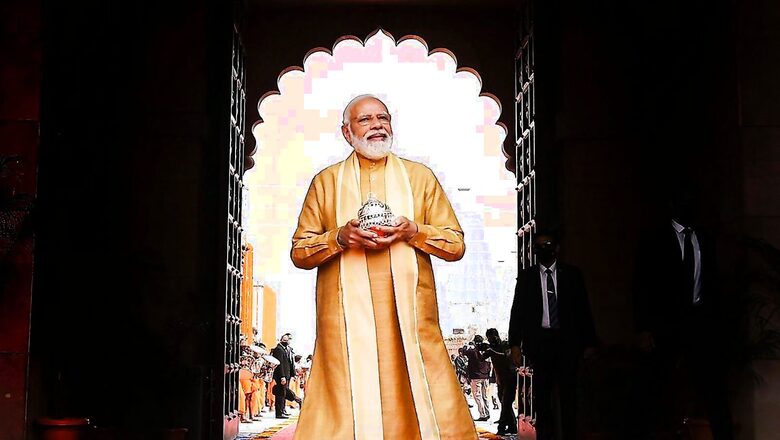
The Narendra Modi government has decided to include more beneficiaries who are not part of the approved Socio Economic and Caste Census (SECC) 2011 database under its flagship health insurance scheme, Ayushman Bharat. It is likely to be included in the Union Budget 2022, which will be presented on Tuesday.
Ayushman Bharat PM-JAY is a scheme implemented in 33 states and union territories across the country, with the beneficiaries identified using the SECC 2011 data. AB PM-JAY is the world’s largest government-funded public health insurance scheme that seeks to provide a cover of Rs 5 lakh per annum each to 10.76 crore poor and vulnerable families (over 50 crore beneficiaries) for secondary and tertiary care hospitalisation. However, till November 2021, the NHA had generated around 17 crore Ayushman Bharat cards — 10.66 crore PM-JAY cards and 5.85 crore state cards to citizens.
According to government sources, Amitabh Kant, CEO of Niti Aayog, had recently told the governing board that the SECC 2011 data was “defective and outdated” and was the primary reason behind the poor uptake of AB PM-JAY.
The governing board of National Health Authority (NHA), then in a meeting held on December 30, approved the proposal to allow non-SECC beneficiaries against SECC family targets in states, UTs. The governing board includes members of Niti Aayog, health ministry, chief health secretaries and additional health secretaries from other states and UTs.
With the approval, new beneficiaries can be identified from other databases and they will be eligible for benefits under the scheme. In the meeting, it was also decided that the state health authorities should try to identify eligible SECC beneficiaries using the 2011 data, but in case of saturation, they could tag non-SECC beneficiaries against the remaining unverified SECC numbers. The board also decided this exercise would be accompanied by issuance of a co-branded Ayushman card.
It was also highlighted that a cabinet note had allowed continuing the use of non-SECC databases in states that have been implementing similar schemes before the launch of AB PM-JAY.
Earlier this month, News18.com had reported that the Modi government was considering extending its programme to around two crore additional families — above the cap of 10.76 crore — and towards this, the NHA may also start considering databases other than the SECC to identify and reach the target beneficiaries.
According to a report by NITI Aayog, ‘Health Insurance for India’s Missing Middle’, around 40 crore citizens – 30% of India’s population – lack access to healthcare protection.
ALSO READ | Ayushman Bharat Set for Reboot With Faster Reimbursement, Incentives for Model Hospitals
Currently, due to severe limitations with the SECC database, only nine states implementing the scheme are relying solely on the SECC database. “Other states/union territories are either using another database or are using SECC along with some other database,” sources said.
In the meeting, it was also discussed how the limitations of the SECC database lead to an increasing preference for non-SECC data sources across the AB PM-JAY ecosystem – from state health agencies to frontline operators, including Arogya Mitra or village-level entrepreneurs.
The board was informed that in the absence of one-to-one mapping of beneficiaries, central share to these states is released on a pro-rata basis.
Further, NHA has also converged various pan-India flagship health insurance schemes for different categories.
Read all the Latest India News here



















Comments
0 comment