
views
X
Trustworthy Source
American College of Allergy, Asthma, and Immunology
National professional organization of allergists, asthma specialists and immunologists that focuses on supporting and publishing research
Go to source
The welts can range from small spots to large blotches that are several inches in diameter. The reaction has many triggers including exposure to foods, medications, allergens, or other substances.[2]
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
By identifying the signs and symptoms, you can recognize and relieve hives.
Recognizing Physical Signs of Hives (Appearance)

Detect itchy or stinging skin spots. Hives may begin as an itchy or stinging area on your skin. If you begin to notice itching, stinging or pain on any parts of your skin with or without a specific cause, it may be hives and you could develop welts. Keep an eye on any itchy or stinging spots for a few days and see if any hives develop. If nothing happens, you may have a bug bite or another condition that caused temporary itching.

Check your skin for welts. Any itching, stinging or pain may quickly turn into welts, which are also known as wheals. You may have individual welt or they may get bigger, spread, and join to form larger patterns of welts or wheals. Welts may be red or skin-colored. Be aware that welts and wheals can appear on any part of your body. They can also change shape and disappear within minutes or hours. Some welts may have a roughly oval shape or be shaped like a worm. They can range in size from a few millimeters to several inches across. See if you have any swelling of the surface of your skin with clearly defined edges, which is a clear sign of hives.

Test for blanching. If you have red welts, press the center of them. If they turn white, this is called blanching. Blanching is a clear sign that you have hives instead of another skin condition. Use gentle pressure when checking for blanching. Pressing too hard may cause swelling or inflammation.
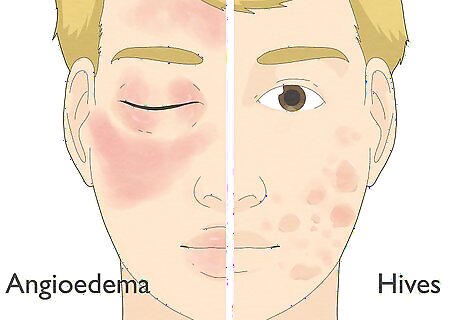
Be aware of the difference between hives and angioedema. Angioedema is a condition that is similar to hives, but it develops in the deeper layers of your skin. It may even occur at the same time as hives; however, there are some differences between the two skin reactions. Knowing what these are can help you get proper care for either condition. Look for angioedema around your eyes, cheeks, or lips. Angioedema most commonly appears in these places. Examine the appearance of any welts you have. If they are large, thick, and firm, they are likely angioedema instead of hives. Feel your welts for pain or warmth, both of which are signs of angioedema.
Identifying the Triggers of Hives (Causes)

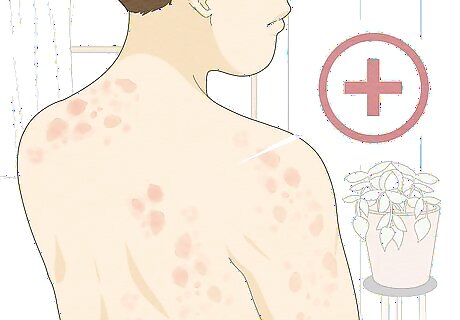
Observe the presentation of hives for potential causes. If you detect hives, they may present on one part of your body or be more widespread. Hives may also always appear on the same spot of your body. Watching the pattern of welts and wheals on your body can help you identify the cause. You may have: Localized hives, which present on one specific part of your body. These hives are generally caused by direct skin contact with food, pet saliva and fur, pollen or plants. Widespread hives, which present all over your body. These hives can be a reaction to a viral infection. They may also be caused by an allergic reaction to food, medication, or an insect bite. Acute hives, which are short-lived. Most acute hives will go away within 24 hours. Chronic hives, which may occur daily for more than six weeks. Each hive will last for less than 24 hours, but others will reappear in different spots.

Recognize the causes of hives. Exposure to different substances may cause hives. Figuring out what may have caused your hives can help you get proper treatment and avoid a more serious reaction in the future — each exposure may increase the intensity of the allergic reaction, especially if a food or medicine is the culprit. The following may cause hives: Foods such as shellfish, fish, nuts, milk, and eggs Medications including penicillin, aspirin, ibuprofen, naproxen and blood pressure drugs Common allergens such as pollen, animal dander, latex, and insect bites Environmental factors including heat, cold, sunlight, water, pressure on the skin, emotional stress, anxiety, and exercise Underlying medical conditions such as lupus, blood transfusions, lymphoma, hepatitis, HIV, and the Epstein-Barr virus.
Be aware of your risk factors. Hives are a very common skin condition. Some people are at an increased risk of developing hives. You may be more susceptible to hives if you: Have had hives in the past Have had other allergic reactions Have a condition associated with hives including lupus, lymphoma and thyroid disease Have a family history of hives.
Dealing with Hives (Treatments)
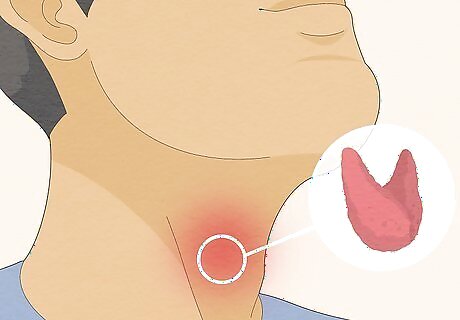
Seek medical attention for severe or recurring hives. If your hives don’t respond to self-care measures or are severe and uncomfortable, call your doctor to schedule an appointment. Your doctor may prescribe medication for your hives or any underlying conditions which may cause them. If you experience angioedema symptoms, a new cough, or a scratchy throat along with the hives, those can be signs the reaction is more serious and you need prompt medical attention. Let your doctor know when your hives started and anything you think may have caused them. Tell your doctor any self-care measures you’ve taken as well. Answer any questions your doctor may have for you. Make sure you mention any food allergies, as some medications and immunizations have food derivatives (such as eggs in flu shots), and should be avoided if you are allergic. Follow any instructions your doctor gives you, including taking prescription medication to relieve the hives. Your doctor may prescribe antihistamines, corticosteroids, autoimmune drugs, or blood protein controllers to relieve your hives.

Clean allergens off of localized hives. If your hives are only on one part of your body, wash the area with soap and water. This can relieve the hives and any discomfort. It may also keep your hives from getting worse. Use a soap of your choice to remove the allergen. Wash the area thoroughly with cool water, which can further soothe your skin. Make sure to rinse the area thoroughly so that none of the allergen remains on your skin. Pat your skin dry with a clean towel to avoid irritating it.

Take a cool bath to soothe your skin. If your hives are more widespread, sit in a cool bath for a few minutes. It can soothe redness and irritation as well as reduce inflammation. Add a few sprinkles of baking soda, uncooked oatmeal, or colloidal oatmeal. These can further soothe itchy and inflamed skin. Stay in the bath for 10 – 15 minutes. Any longer and you might get too cold.

Dab on calamine lotion or an anti-itch cream. Hives often come with intense itching and inflammation. Gently rubbing a calamine lotion or non-prescription anti-itch cream can soothe itching and inflammation. It may also relieve your hives. Purchase either calamine lotion or a nonprescription hydrocortisone, or anti-itch cream. Get an anti-itch cream that is at least 1% hydrocortisone. Put on the calamine or hydrocortisone to the affected area once a day after you bathe.

Take an over-the-counter antihistamine. If your hives are widespread, take an antihistamine. It can block the histamine that is causing your hives and relieve itching and inflammation. Be aware that antihistamines can cause drowsiness. Follow dosing instructions on the following anti-histamines for optimal effects: Loratadine (Claritin) Cetirizine (Zyrtec) Diphenhydramine (Benadryl, others)

Apply cool, wet compresses. The itching and inflammation associated with hives are a result of histamine in your blood. Apply a cold pack or cool, wet compresses to alleviate itching and inflammation. This can also prevent you from scratching Cover your hives with compresses for 10 to 15 minutes. You can apply them every two hours or as needed.

Avoid scratching hives. Even though hives can be very itchy, it’s important to not scratch them. It can spread allergen over a larger area of your skin and make symptoms worse. It can also lead to other problems such as a skin infection.

Wear loose, smooth-textured clothing. Some types of clothing can irritate hives. You can prevent and relieve itching and inflammation by wearing loose clothing that has a smooth texture. Clothing that covers your hives may also protect your skin from triggers and relieve symptoms. Choose clothing made of cotton or merino wool. This can prevent scratching and excess sweating, both of which may make your hives worse. Consider long-sleeved shirts and long pants to protect your skin from external irritants.

Stay away from triggers. Hives often develop as a result of an allergen or specific irritant. If you know what your trigger is, try and avoid it. If you don’t, rule out the cause by limiting exposure to suspected triggers. Remember that your trigger could be an allergen such as pet dander, a food allergy, a topical product such as detergent, or an environmental factor like sunlight. Limit your exposure to suspected triggers. If this relieves your hives, you’ve likely found your specific trigger. Keeping track of things such as what you eat, wear, cleanse with, and are exposed can help you point out your triggers. Be aware that sun exposure, stress, sweat, and temperature changes can cause and exacerbate hives. Wash with mild or “hypoallergenic” soaps and detergents. These have fewer chemicals that may cause hives or make them worse.



















Comments
0 comment