
views
X
Trustworthy Source
National Health Service (UK)
Public healthcare system of the UK
Go to source
Arthritis occurs when your joint becomes inflamed, causing pain, stiffness, and swelling. Osteoarthritis happens when the cartilage in your joint wears away, while rheumatoid arthritis is an autoimmune condition where your body attacks your joints. Experts say arthritis in the knee is very common because it's a weight-bearing joint, but you can get arthritis in any joint.[2]
X
Research source
Although arthritis may interfere with your life, you may be able to manage your condition.
Dealing with Knee Arthritis at Home
Lose weight if you're too heavy. As a general rule, people who are overweight or obese suffer more arthritis because of the increased amount of pressure on their joints — especially weight-bearing joints such as the knees, hips and low back. Furthermore, overweight people are more likely to have flat feet and fallen arches, which promotes "knock knees" (also called genu valgum). Genu varum is hard on knee joints because it causes misalignment of the thigh (femur) and shin (tibia) bones. Thus, do your knees a favor by losing excess weight. The best way to lose weight is by increasing cardiovascular exercise (such as walking or cycling) while decreasing your daily calories at the same time. Most people who aren't especially active only need about 2,000 calories daily to maintain their body processes and still have enough energy for some exercise. Reducing your daily caloric intake by only 500 calories can result in about 4 pounds of lost fat per month. Swimming is a fantastic exercise for arthritis sufferers to lose weight because your body is buoyant and no pressure is put on your joints.
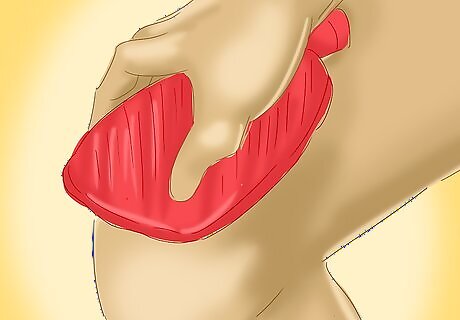
Use moist heat for osteoarthritis. Osteoarthritis (OA) involves some inflammation, but not nearly as much as either types, such as rheumatoid arthritis (RA), gout attacks or psoriatic arthritis (PA). Instead, OA involves wearing out of the knee cartilage, formation of bone spurs, grating sensations, pain, loss of flexibility and stiffness, particularly first thing in the morning after many hours of disuse. As such, moist heat is a much better choice for OA instead of ice because the warmth dilates blood vessels (larger diameter) around the knee, improves circulation, loosens up muscles and helps to alleviate joint stiffness. Apply moist heat first thing in the morning or after not using your knee for long periods of time. Avoid electric heat sources because they can dehydrate the skin and muscles around the knee. Microwaved herbal bags work well for knee arthritis, especially the ones that are infused with aromatherapy (lavender, for example) because they tend to have relaxing properties. Consider soaking your legs (or entire lower body) in a warm Epsom salt bath, which can significantly reduce stiffness and pain, especially within the joint and surrounding muscles. Nearly 30 million middle-aged and elderly Americans have been diagnosed with OA somewhere in their body.
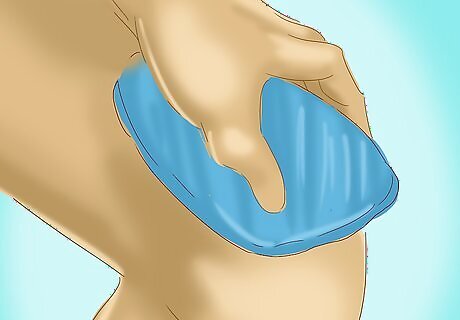
Use cold therapy for inflammatory arthritis. Using cold therapy, such as crushed ice, ice cubes, frozen gel packs or veggies from the freezer, is much more appropriate and effective for inflammatory types of arthritis that involve severe swelling and redness. Cold therapy causes blood vessels to constrict (smaller diameter) and reduces the amount of blood flowing to an area, which helps to control inflammation and pain. Gout, RA, and PA can all affect the knee and typically create considerable throbbing pain and disability — making it very difficult to walk and impossible to run. Some form of cold therapy should be applied to your inflamed arthritic knee(s) on a regular basis, especially after any sort of exercise, for 10–15 minutes or until your knee(s) feels numb to touch. Start with two to three per day and increase from there if it seems to be helpful. Always wrap crushed ice or frozen gel packs in a thin towel before placing it around your knee in order to prevent frostbite or skin irritation. The best places to put the cold therapy is on the front and sides of the knee, which is close to where the joint space and inflammation is. Inflammatory types of arthritis are more common in the elderly, but they also afflict younger adults and even children.
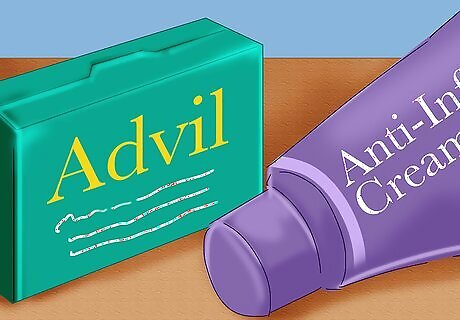
Take non-steroidal anti-inflammatory drugs (NSAIDs). Consider taking over-the-counter NSAIDs, such as ibuprofen (Advil, Motrin), naproxen (Aleve) or aspirin for short-term relief of pain and inflammation. However, these medications can be hard on your stomach and kidneys, so it's best not to rely on them for longer periods of time — much more than a few weeks. It helps to take NSAIDs with food (on a full stomach), preferably non-acidic varieties, to reduce the risks of stomach irritation and ulceration. Alternatively, some over-the-counter painkillers such as acetaminophen (Tylenol) are effective for mild-to-moderate knee arthritis, but they don't reduce inflammation. Pain relievers (called analgesics) can be hard on your liver and kidneys, so always follow recommendations. Pain relieving creams and gels applied directly to your arthritic knees is another option, and one that's better for your stomach. Capsaicin and menthol are natural ingredients found in some creams that distract your brain from pain by making your skin tingle.

Get regular exercise. Some exercise for your legs is important because the muscles around your knees sort of act as secondary shock absorbers for the joints and help reduce impact. Thus, the stronger the muscles surrounding your knee joints (thigh, hamstring and calf muscles), the more stress or impact they can absorb or dissipate. However, not all exercise is appropriate for your knees — high impact exercises such as jogging, running, tennis and climbing stairs will make arthritic knees worse. Stick to walking and cycling, either outside if weather permits or at your local gym Gym exercises that increase quadriceps (thigh muscles), hamstring and calf strength without inflaming knee joints include mini-squats, leg presses and leg extensions. These leg exercises should be pain-free and done with limited knee flexion — not greater than 45 degrees. Some exercise, at least walking, should be done every day. If going to the gym is your thing, then aim for three times weekly. Switch from high impact activities to swimming and water aerobics in the pool. The buoyancy of the water reduces the stress on your knees, but still works out your leg muscles.
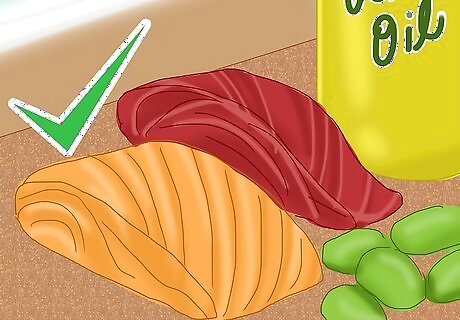
Eat more foods rich in omega-3 fatty acids. Dietary factors play a role in either irritating or helping soothe arthritis. Diets high in refined sugars tend to make arthritic pain worse, whereas diets rich in omega-3 fatty acids have a mild-to-moderate anti-inflammatory effect on the body. Omega-3 fats can be particularly helpful for controlling the pain of RA, but not for slowing its progression. The three omega-3 fatty acids found in food are called ALA, EPA and DHA. Unfortunately, the standard American diet tends to be low in omega-3 fats and too high in inflammation-promoting omega-6 fats. Fish, plants and nut oils are the main dietary sources of omega-3 fats. EPA and DHA are found in cold-water fish (salmon, mackerel, tuna), whereas ALA is found in flaxseed oil, canola oil, soybeans, hemp seeds, pumpkin seeds and walnuts. If supplementing with fish oils or seed-based oils to get omega-3 fatty acids, aim for 1,000 mg 2-3X daily for noticeable anti-inflammatory effects.

Consider taking glucosamine and chondroitin supplements. Glucosamine and chondroitin sulfate are substances naturally found in all joints. Glucosamine essentially acts as a lubricant, whereas chondroitin allows the cartilage to absorb more water and be a more effective shock absorber. Both compounds can be taken as supplements, and although the research is somewhat mixed, the evidence suggests that they can be helpful for reducing the pain of all types of arthritis — particularly large weight-bearing joints such as the knee. Glucosamine can also increase mobility in mild-to-moderate cases of OA, especially in large weight-bearing joints such as the knees. Glucosamine sulfate is often made from shellfish, which can lead to allergy concerns, so be cautious when supplementing with it. Glucosamine hydrogen is made from vegetable sources, but may not be as effective compared to the sulfate type. An effective dose for arthritic knees is about 500 mg three times daily, but it often takes two to four months to get noticeable results.
Seeking Medical Treatments

Get stronger prescription medications from your doctor. Make an appointment with your family doctor to confirm if you have arthritis in your knees. Your doctor will likely take x-rays and blood tests to confirm a diagnosis of OA, RA or other types of arthritis, such as gout. If the arthritis is causing lots of pain and stiffness, over-the-counter medications may not be strong enough to lessen the symptoms. In such cases, your doctor will likely prescribe stronger anti-inflammatories. COX-2 inhibitors (celecoxib, meloxicam) are strong types of NSAIDs that may cause fewer stomach problems. They are commonly prescribed for OA of the knee. Disease-modifying anti-rheumatic drugs (DMARDs) are commonly used to deal with the pain and slow the progression of RA by reducing an overactive immune system. DMARDs include methotrexate, sulfasalazine, hydroxychloroquine, etanercept, and adalimumab. Classic signs of arthritis on x-ray are: loss of joint space due to thinning cartilage and bone spurs that stick out from the femur or tibia bones.
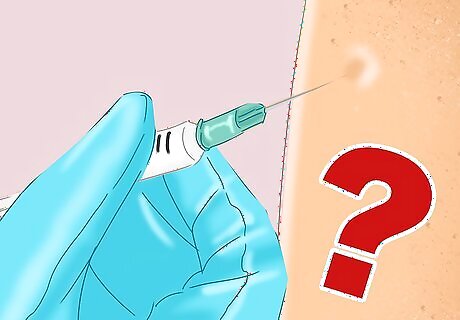
Ask your doctor about steroid injections. An injection of corticosteroid medication (cortisone) into a knee joint can quickly reduce inflammation and pain, and allow normal movement of the joint pretty quickly. Corticosteroids are hormones that display powerful anti-inflammatory properties and are made by the body's adrenal glands. They are injected by an orthopedic surgeon under anesthesia. The most commonly used preparations are prednisolone, dexamethasone, and triamcinolone. The effects of the medications are short-term — lasting from weeks to months typically. The number of cortisone injections you can get each year is limited because it can worsen knee joint damage over time. Potential complications of corticosteroid knee injections include local infection, excessive bleeding, tendon weakening, local muscle atrophy and nerve irritation/damage. Steroid injections can be relatively expensive if your insurance doesn't cover it.

Consider infrared therapy. Using low-energy light waves (called infrared) is known to be able to speed up wound healing, decrease pain and decrease inflammation in a variety of joints, including the knees. Use of infrared radiation (via a hand-held device or within a special sauna) is thought to penetrate deep into the body and improve circulation because it creates heat and dilates (opens up) blood vessels. Furthermore, there are virtually no negative side effects of infrared therapy. In most cases, significant knee pain reduction occurs within hours after the first infrared treatment, which lasts between 15 and 30 minutes per session. Pain reduction ranges from 40% to 100% better after treatment and is often long lasting — weeks or even months. Health professionals most likely to use infrared therapy on joints include some chiropractors, osteopaths, physiotherapists and massage therapists.
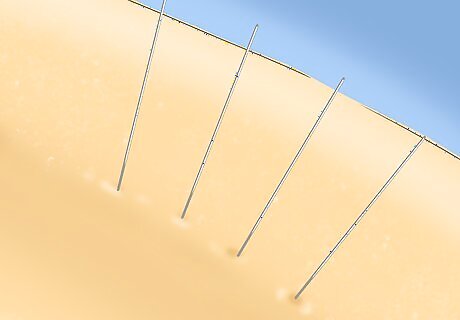
Try acupuncture treatments. Acupuncture therapy involves sticking thin needles into specific energy points within your skin/muscle in efforts to decrease pain and inflammation and to potentially stimulate healing. Acupuncture is gaining popularity as an arthritis therapy and some studies indicate that it can relieve pain and improve function in people with OA of the knee. Acupuncture is relatively painless and has an excellent safety record — the only risks are local bruising and infection. It seems to be worth a try if your budget allows for it, as it isn't covered under most health insurance plans. Acupuncture is based on the principles of traditional Chinese medicine and alleviates pain and inflammation by releasing the hormone serotonin and other substances called endorphins. Acupuncture is much more mainstream now and practiced by a variety of health professionals including some medical doctors, chiropractors, naturopaths, physiotherapists and massage therapists — whoever you choose should be certified by NCCAOM.

Consider surgery as a last resort. If conservative home-based remedies and non-invasive treatments from your doctor aren't effective at reducing the symptoms of your knee arthritis, then surgery may have to be considered. Surgery should only be done in severe cases of arthritis where the knee joint is severely damaged and all other modes of treatment have failed. There are many types of surgical replacements, ranging from minor arthroscopic surgery to complete knee replacement surgery. Surgery is more common for advanced OA and not as common for inflammatory types of arthritis, unless the cause is clearly understood or the entire knee joint is destroyed. Arthroscopic involves inserting a small cutting instrument with a camera attached into the knee to clean up pieces of torn cartilage. Recovery time is quick — a week or two, depending on the extent of the damage. Cartilage grafting involves adding healthy cartilage to a damaged knee meniscus. This procedure is usually considered only for younger patients with smaller areas of damaged cartilage. A synovectomy involves removing the knee joint lining that's been inflamed and damaged by RA. An osteotomy involves reshaping or sanding down the leg bones that form the knee joint — the tibia and/or the femur. An arthroplasty is a total or partial knee replacement. The damaged cartilage and bone is removed and replaced by an artificial knee joint made of metal and plastic. This surgery is the most invasive and takes the longest amount of time to recover from.



















Comments
0 comment