
views
As the world battles the Covid-19 pandemic, medical fraternity is racing against time to evaluate the efficacy of the screening tests available. However, it's also imperative to understand how the SARS-CoV-2 is raging a war against the human body.
A virus is a single or double-stranded nucleic acid (RNA or DNA) enveloped by a protein membrane. The club-shaped glyco-protein spikes give the Covid-19 virus a crown-like shape similar to that of the sun’s corona, hence the name coronavirus.
A virus is not a living object in the real sense as it cannot reproduce by itself. Thus, it seeks a way around this innate reproductive deficiency by attaching itself to a healthy cell. It soon takes control of the entire cell function. The cell mechanism is then utilised by the pathogen to create multiple copies, resulting in either the host or the infected cell getting damaged/killed in the process.
The presence of an alien element in the tissues raises an alarm in the immunity system of the infected person. This triggers a defence mechanism by way of production and release of virus-combating antibodies in the body.
So, there are broadly two ways to find out if a person has indeed been exposed to the virus —— the presence of the virus itself or the detection of antibodies which the body may have developed to fight the foreign agent.
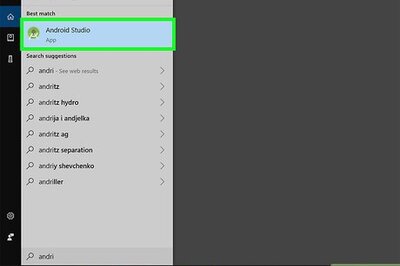
Reverse Transcriptase-Polymerase Chain Reaction or RT-PCR is the most commonly used confirmatory test to identify Covid-19 cases.
The test reads the presence of virus Ribonucleic Acid (RNA) in a throat or nasal swab to detect if a patient has been infected with the pathogen.
Another process to test a Covid 19-positive patient is through what is called Virus Antigen Test. This process identifies the virus protein enveloping the RNA.
Though both RT-PCR test and viral antigen test can be utilised for early detection of the disease, the former is said to be more sensitive.
“RT-PCR test is more sensitive because in detecting the virus, the nucleic acid is amplified many times over to detect the presence of the microbe. Antigen tests measure only the load of virus protein that is there, although the detection signal can be amplified a bit,” says Dr Gagandeep Kang, executive director of the Transnational Health Science and Technology Institute, Faridabad.
Despite being a highly sensitive test, sometimes even the RT-PCR tests may fail to detect the presence of virus in a sample. Research shows that swab collected from one in every five patients may give a false negative result.
Professor Leo Poon from the School of Public Health, Hong Kong University attributes these anomalies to a possible low virus load in a sample collected for testing.
“Take the example of fish in an aquarium. If there are many fishes then there is no problem in taking a sample of the fish. So if the patient sample has a high viral load, the probability of catching the virus in the sample is high. Lower the number of virus in the sample, the lesser chance you would be able to get the test positive,” Professor Poon explained during a workshop for journalists earlier this month.
But both tests are important in early detection of the disease and to reduce its spread as Covid-19 patients shed large amounts of the pathogen in the first week of being exposed to the virus. In some cases, the patients have shown transmissibility even before the onset of clinical symptoms. Which renders them mobile and infectious.
Between RT-PCR and Antigen test, the former is the preferred method for the detection of the virus.
“You may miss a lot of patients if you use this test (Antigen test) to detect at an early stage. If the patient is tested negative, they may be sent home and then they can spread the virus to other people,” says Leo Poon, Professor School of Public Health, Hong Kong University.
The second method to test for Covid-19 is by checking for the presence of antibodies in the blood sample of a patient. Also called serological test, this process takes lesser time than the RT-PCR test.
Serological tests detect the presence of antibodies generated by the body’s immune system to fight the disease. The presence of antibodies may get registered only a week after the exposure to the virus and hence this process is generally used for surveys to estimate the spread of the disease in a community.
“Serological test is likely to be positive after the immune system of the infected person has started to produce antibodies. That may take seven to nine days after exposure to the virus. The RT-PCR test, on the other hand, can detect the virus at an early stage of the infection, even just before symptoms start,” says Dr Kang.
Since it takes lesser time to conduct serological tests, they are considered useful in assessing the spread of the disease, surveys, and determining mathematical models to predict the impact of pathogen spread over a period of time.
For instance, ICMR used antibody tests in the first week of May to estimate the growth on infections in hot spots and major cities.

















Comments
0 comment